This is a placeholder for the Yext Knolwedge Tags. This message will not appear on the live site, but only within the editor. The Yext Knowledge Tags are successfully installed and will be added to the website.
,
This is a placeholder for the Yext Knolwedge Tags. This message will not appear on the live site, but only within the editor. The Yext Knowledge Tags are successfully installed and will be added to the website.
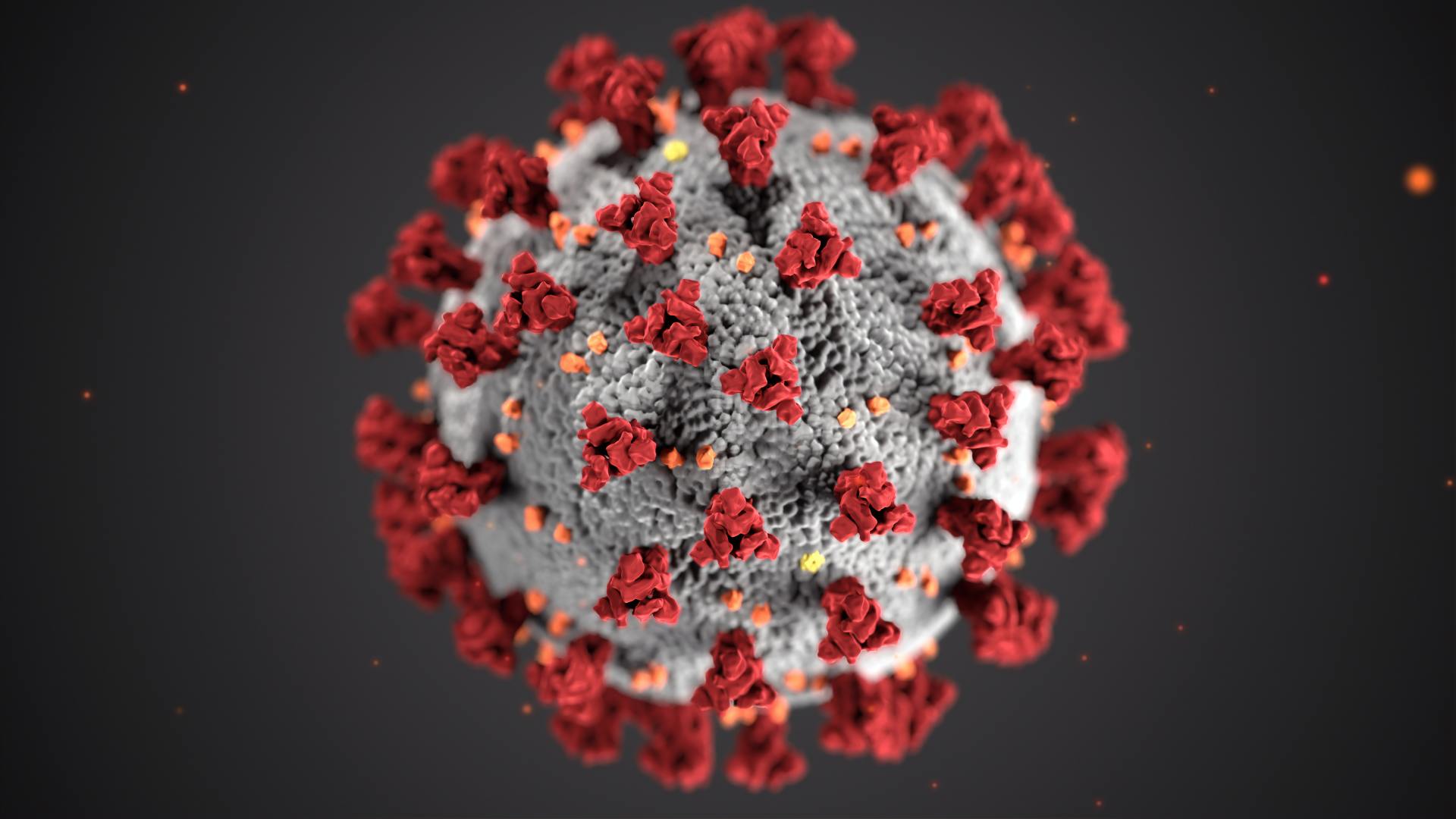
COVID-19 UPDATE - Masks are no longer required in the office, but temperature checks are still done. If you are sick or have been around someone who may have COVID - please let us know BEFORE coming in.
,
This is a placeholder for the Yext Knolwedge Tags. This message will not appear on the live site, but only within the editor. The Yext Knowledge Tags are successfully installed and will be added to the website.
Diabetes – Diabetic Neuropathy and Tips for Healthy Feet
Hibu Websites • Feb 21, 2020
What is Diabetic Peripheral Neuropathy?
Diabetic Peripheral Neuropathy (DPN) is nerve damage that is caused by high blood sugar and triglycerides. It is unfortunately very common and up to half of all people with diabetes may struggle with diabetic peripheral neuropathy. DPN can cause people to have both pain and numbness and lead to severe problems like ulcers, bone infections, and even amputations. It can also cause problems with balance, problems walking, decrease muscle tone and lead to structural changes in feet. People may not always be aware that they can’t feel their feet enough to protect them – and this is why it is essential to have a diabetic foot exam at least once a year.
Pain
People with DPN have a burning, tingling, pins and needles sort of pain that is often worse at night or after being on their feet a lot. It is usually symmetrical and progresses from the toes up the legs over time. After a while, it can also affect the hands.
Numbness
If you can’t feel your feet, then it is harder to protect them. People with diabetes have problems sensing pressure, pain, and temperature at times. This can lead to foot sores developing. These sores can develop by stepping on something, friction or other causes. Once established they are then often hard to heal and have a higher risk of infection if the person’s blood sugar isn’t controlled. If the person is a smoker or has peripheral vascular disease, it can be especially hard to heal.
Sometimes people can have so much numbness that they may not be able to feel if they have a broken bone in their foot. This can lead to them walking on it and developing a problem called a Charcot foot – which could need surgery or even lead to amputation.
Unusually shaped feet may not fit right in shoes, which leads to an increased risk of ulcers and adverse outcomes. DPN can lead to other structural changes feet which can make it more common to get ulcers. Once people have one ulcer, they are more likely to get another one. If these sores aren’t tended adequately they can get infected, this infection can spread to the bone and lead to amputation. Treatment may involve removing dead/infected skin, staying off feet, using a special brace to care for it. Frequently patients will be under the care of a podiatrist or a wound care clinic to help care for foot sores. If your PCP refers you to one these specialists – please go!
Treatments:
While DPN can be very painful, there are treatments which your doctor may recommend for this nerve pain. Antidepressants – like amitriptyline or duloxetine, anticonvulsants – like gabapentin or pregabalin are effective and reducing pain and increasing function for people dealing with DPN. Physical therapy can help with strength and balance, and bed cradles can be used to keep blankets off feet during the night.
Tips for healthy feet:
- Inspect your feet daily – use a mirror or ask someone to help if you can’t see. Check your whole foot – big toes, little toes, the ball of the foot, sides of foot, heel…
- Bathe feet in lukewarm water every day
- Moisturize feet – but not between toes. Extra moisture can lead to infection. Feet can become drier because the nerves that control the oil/moisture in your feet aren’t working right anymore.
- Cut nails carefully – straight across, file edges if needed.
- DON’T cut corns/calluses yourself – talk with your family doctor or podiatrist about it. If not appropriately treated these can turn into sores.
- Wear clean, dry socks – maybe diabetic socks.
- Wear socks and shoes all the time. Don’t walk barefoot
- Protect feet from hot and cold – wear shoes on the sand/sidewalk, test water with fingers before getting in the tub, no hot water bottles or heating pads to your feet.
- Look and feel in shoes before putting your feet in. You could walk all day with a pebble in your shoe and injure your foot without knowing it.
- Consider special shoes or orthotics – Buy them later in the day when feet are larger and break them in slowly.
- Stop smoking – smoking damages blood vessels and makes it harder to heal and dramatically increases your chance of amputation.
***Note *** This post, like all my other posts, is for general medical information only and is not to be taken as direct advice. Please consult your personal physician for more information.

By Cynthia Villacis, MD
•
24 May, 2020
Happy Memorial Day! It has been over 2 months since the quarantine started here in KY. It has been quite a rollercoaster of emotions and a mixture of experiences - both had and missed. It has touched everyone to some degree - whether it be physically, emotionally, or financially. In my family, both of my children had graduations that were supposed to happen - which didn’t happen in the traditional sense - and never may. My daughter’s graduation was changed to an alternative one where there are groups of 28 teens in cars with their families. We will be going to 3 different parking lots to hear the principal’s speech, get a picture taken in cap and gown and then hearing the class president’s speech where they will turn their tassel. My parents will not be able to be there in person, graduation parties won’t be celebrated the same way and the class of 2020 won’t be together again - unless they are allowed to go ahead with their group graduation - which is tentatively scheduled for July or August at the college arena. I am not feeling hopeful. We did get to decorate a door for her, submit an ad for the yearbook, attend Obama’s graduation ceremony, and have gotten her family presents. Not sent out are the invitations from Josten’s to family members - although I am tempted to scratch out the original plans and write in the alternative ones as a comment on the times. My son decided to skip his Bachelor’s graduation last year and was going to just go to his Master’s graduation ceremony this spring. But that obviously was canceled or rather postponed until December. He is one of the lucky graduates who has a job that still wants him to start on time and he has moved to DC, and will be starting his new position this week. If his graduation ceremony does actually happen in December, will he or his classmates who have scattered to the wind come back for the ceremony? Or as I suspect, will they have moved on to the next stage in their lives… Both my husband and I have been blessed with the ability to continue to work during this time when so many were furloughed or lost their jobs. I am thankful for not being in the position so many are in - having to try to figure out how to pay a mortgage or health insurance without having a job. I know some people who didn’t qualify for unemployment payments because they hadn’t been able to work enough hours the previous year, or because they were students and their jobs weren’t designed to be permanent positions. I know others who are making more money by being furloughed and getting the government benefits of $600/week in addition to their unemployment insurance than they ever did while they were employed. I know others who have been deemed “essential” and stayed at work for close to the minimum wage - and risked being exposed to the virus so that they could support themselves and their families. This health pandemic has again brought up the health insurance debate. What happens to health care when insurance is tied to employment and that employment goes away? I choose to work outside of insurance by charging an accessible monthly membership - primary care is available this way regardless of employment status - but it doesn’t cover hospitalizations, ER visits, etc. In an age of large hospital systems, I was reduced to buying masks and cleaning supplies on Amazon and eBay at very inflated prices since I hadn’t bought enough from traditional medical retailers in the last few months and they were allocating these based on prior purchases. I have been able to easily ensure social distancing since my office is low volume by design. I was able to easily pivot and offer Telehealth visits because I am an independent practitioner and I had already been doing some of these since I opened my DPC office several years ago. My lease is up this month and I am considering relocating to a more economical location for the next few years. Lacking sufficient PPE, Danielle has been working from home for the last few months. Like all other small businesses, we have had to pivot. No matter your financial situation, the COVID-19 pandemic has taken a toll on all of us emotionally. People who are at increased risk from dying from the virus due to age or health status are scared, feel isolated and are hurt that people are refusing to wear masks because they don’t like them, don’t think they will get sick or because they are upset that the government has closed down the economy and is telling them what to do. People who haven’t known anyone who has been infected with COVID-19 and/or live in areas where much economic damage has been done by the closures, are upset by all the restrictions that have been in place and the effect that it has had on their quality of life. Being in isolation for several months is really hard. I think no matter our political party or personal situation, we would all like to believe it to be true that we can go back to our regular way of life soon. But wanting something to be true, doesn’t necessarily make it so. As we proceed to open up our economies, more people will get sick. The point of the shutdowns was to “flatten the curve” but even a flat curve has new infections - just not to the degree that they are crippling our medical systems’ ability to handle them. It is a very delicate balance trying to balance people’s emotional and financial health with their physical health - when you have a virus that can be in someone for up to 2 weeks before they get sick, if they get sick at all! The flattening has bought us time to get more PPE, work towards developing a vaccine, and learn a little more about the best way to treat it - although much is still controversial and much work remains to be done. The next test is how people will respond as we reopen. It is my hope that people will wear masks and still take some precautions to avoid spreading the virus. If everyone does this out of respect for each other and the workers who are unable to avoid customers who aren’t wearing masks - then fewer people will get sick and possibly lose their lives, and businesses will have a much better chance of staying open and the economy will have a better chance of staying up and running. If you are having trouble using a mask I would suggest you watch one of my recent videos on “Mask Wearing 101”. If you are not wearing a mask out of personal preference, I would ask that you reconsider. My last blog post was almost 2 months ago when we were just at the beginning of this. And as I predicted - much has changed in this time. At that point in time, there weren’t any confirmed cases of COVID-19 in the greater Cincinnati area. As of today, according to the Hamilton County and Northern Kentucky Health Departments, there have been 3,462 confirmed cases here. I am sure that there have been many more people who have had it than that though. Testing has been an issue - many people were told initially that they weren’t sick enough to get tested and the only people getting tested were those who were sick enough to possibly get admitted or if they were healthcare professionals. Also, many people probably have had it and haven’t been aware of it since not everyone develops symptoms. I am thankful that we haven’t seen the extent and severity of disease that others have seen in other areas of the country and world and I hope and pray that our leaders show wisdom as they guide us through this next phase of the COVID-19 pandemic, and that they are able to find a balance between apparently competing interests. I pray that we are able to come together as a people and fight the virus instead of each other, and through being united move through this period with as little damage to our health, economy and psyches as possible.
By Dr. VIllacis
•
11 Mar, 2020
What is it? The Coronavirus 2019, or “COVID-19” is caused by a virus known as SARS-CoV-2. It appeared in late 2019 in the city of Wuhan, China and is now on every continent outside of Antartica. See this global map on the CDC website for current countries impacted: https://www.cdc.gov/coronavirus/2019-ncov/locations-confirmed-cases.html#map Most people who get sick do recover, but it is more likely to kill than the regular flu. It is not just a bad cold. The regular flu has a mortality rate of 0.1% - whereas COVID-19 has an average mortality rate of around 2%. The risk of death from the virus raises with age and serious medical problems like COPD, kidney disease, diabetes and heart disease and may be up to 15% in some cases. That said, most people who get sick do recover - even if they end up getting hospitalized in the process. How is it impacting us? As of 859-905-0707, there haven’t been any confirmed cases of COVID-19 in the Greater Cincinnati area. However, it is no longer considered to be a question of IF we will see the virus in our community, but rather WHEN. The nearest confirmed cases are in Cynthiana, KY - which is about an hour away. That said, the region has already started to feel some impact from the virus. Many colleges have suspended in-person classes, masks and hand sanitizer are not available to purchase, and the City of Cincinnati just declared a State of Emergency and is recommending that large events cancel themselves. What symptoms do people have? That is tricky - it may be none, or like a cold or the flu, or a pneumonia that you can take care of at home; - or it may end up in hospitalization or even death. People infected with COVID-19 may not have any symptoms until 2-14 days after they catch the virus - the average being 5.3 days. The most common symptoms include some combination of: Fatigue Muscle Aches Fever (meaning >100.4 oral) Cough Trouble Breathing One common presentation is a week of low-grade flu-like symptoms followed by shortness of breath and pneumonia. Do I need to be seen? The answer is maybe. If you have life-threatening/severe symptoms - call 911 or go to the ER. If you don’t and you are my patient, please call me or message me on Spruce so we can talk about what the next best step is. The next step will depend on your symptoms, medical history and the chance that what you have is COVID-19 instead of another illness. As of today - risk factors are considered to be: recent travel to China, Italy, Iran, South Korea, Japan and unofficially Egypt, having known close contact with someone who has tested positive for or is suspected to have coronavirus or being a healthcare worker. If after we talk, I am concerned that you may have COVID-19, then I will next contact the Kentucky Department for Public Health for further instructions. If the Kentucky Health Department feels there is a need then they will authorize the test and you will be referred to the appropriate emergency department for testing. Please, DO NOT just go to the ER on your own unless you are having severe symptoms. There are not enough tests at this point in time for everybody who just wants to make sure they don’t have it to get checked, AND if I DO think you may have COVID-19 - the ER needs to be given advance notice so they can decrease the chance of your exposing other patients and staff to the virus. The COVID-19 test, if you need it, usually involves taking samples of fluid from the inside of your nose and mouth. Current recommendations are that this specimen collection needs to occur in a negative pressure environment - which is only available at the hospital. It may also involve testing a sample of mucus that you cough up or a chest x-ray. Getting evaluated may also involve testing for other illnesses like the flu or strep throat - since if you have one of those it is very unlikely that you also have COVID-19. How is it treated? Most people are able to stay at home and take over the counter medicines to manage their symptoms. There is not a cure for COVID-19, nor are there specific medicines to treat it. Antibiotics or Tamiflu don’t work. It is also advised to stay in one room of their house and use a separate bathroom from others if at all possible. Please make sure to read recommendations on cleaning and disinfection especially if you have someone sick in your household. https://www.cdc.gov/coronavirus/2019-ncov/protect/index.html It is important not to go out into the community again until they are all better. In more severe cases people can require oxygen or even be put on a machine to help them breathe, called a ventilator. Can I keep from catching it? While there is no vaccine to prevent it, there are things you can do to decrease the chances of getting COVID-19. Wash your hands with soap and water often and thoroughly (sing “happy birthday” twice and make sure to wash all surfaces and under nails) Use hand sanitizer if no soap/water is available Use approved cleaners to clean surfaces at work and home - there are reports the virus may live on surfaces over a week. Don’t touch your face. Stay at least 3-6 feet away from others - especially anyone coughing or sneezing. Avoid large gatherings of people. Don’t travel to areas where there are known to be a lot of cases of COVID-19. Avoid mass transit and cruise ships if possible. If you are caring for someone who is sick have them wear a mask and wear one yourself. Be very careful of how you remove it and wash your hands afterward. The CDC recently recommended that those over 60 or those who have underlying immune problems decrease the face to face contact they have with others to decrease the chance of getting the disease. Please keep this in mind when you are deciding what to do. See their link for more information https://www.cdc.gov/coronavirus/2019-ncov/specific-groups/high-risk-complications.html?fbclid=IwAR0H3PZa5tlPA3ZGX0M7AWUaFViX9KFY4i1K0eYZg_utKogcI3dRTtjSAl0 What can I do to prepare? If you are able to get a 3 month supply of medications to decrease the number of times you have to go to the pharmacy and in case there is a disruption in the supply chain. Make sure you have over-the-counter medicines you would use for the flu at home. Have at least a 2 week supply of household items and groceries on hand so you can stay home if you need to or in case there is a shortage of items in the community. https://www.cdc.gov/coronavirus/2019-ncov/protect/index.html What is Health Connections DPC doing differently? For starters, we have started asking more triaging questions when people call to schedule appointments. We are contacting our patients who have scheduled appointments and per CDC recommendation encouraging them to be conducted via telemedicine if appropriate. And I am staying in contact with my colleagues across the country to get ideas and be aware of best practices, and paying attention to local communications from the hospital systems and health departments. And I am praying. Summary This is likely to be a rapidly changing situation and recommendations may come from the CDC, Health Department or World Health Organization or other healthcare bodies. Things mentioned on this page may no longer be true by the time you read it! I would encourage you to become familiar with the CDC website page for COVID-19 and to pay attention to guidance from local officials regarding caution with attending large gatherings. Even though there are only 8 cases in KY now, there are probably many more that haven’t been detected yet or are mild enough that they weren’t tested. By decreasing our exposure, we can minimize the spread of the virus and decrease the chance that we or our loved ones are infected. Although the unknown about this situation can be scary, please don't be scared. Just prepared.

By Hibu Websites
•
21 Feb, 2020
Hi! I’m Cynthia Villacis, and I have been practicing Family Medicine for the last 14 years. While I have learned a lot over this time, one thing I have not learned well, is to stay on time with the 15 minutes I have been given to see you. Honestly, most doctors struggle with this. The only way NOT to do this is to limit visits to 1-2 concerns at a visit, and not deal with complex patients or mental health issues. This also leads to you having to come back to finish the visit another day, or to me running behind. While most of my patients tell me they don’t really mind waiting because they know I care and will take the time with them if they need it, I always wonder – I mean who really WANTS to wait at the doctors office? Wouldn’t it be better for both of us if I could just schedule longer appointment times? Unfortunately, as an employed physician I am not in charge of my schedule – and administration hasn’t allowed me to do this. I was feeling frustrated about this last summer when I found out about Direct Primary Care. Direct Primary Care is a new model of providing healthcare for a monthly membership fee. It is not the same as concierge medicine. By paying a monthly fee that is less than a cable or cell phone bill and still NOT charging your insurance, I will be able to lower my overhead, have visits with you for 30-60 minutes instead of 15, address some issues over the phone if we both want to, and keep medical decisions between you and me. I will be able to provide discounted generic medications (not controlled substances) and refer patients for labs/tests at reduced prices. This model works great for someone with a high deductible plan who typically doesn’t meet their deductible, someone who doesn’t have insurance, or someone who wants to have less rushed visits with their doctor and better access to them. I went to a conference on Direct Primary Care with my husband in October and what I learned there, coupled with ongoing support from some awesome mentors on Facebook, has led me to believe that this is the best way for me to practice medicine. I have resigned from my regular practice effective February 28, 2017 and will be focusing my efforts on opening a practice on my own. I am still searching for an office location in Kenton County but am planning on opening my family medicine office in the next several months. I am very excited, and a little nervous, about making this leap but have confidence that this change will be a win-win!
By Hibu Websites
•
21 Feb, 2020
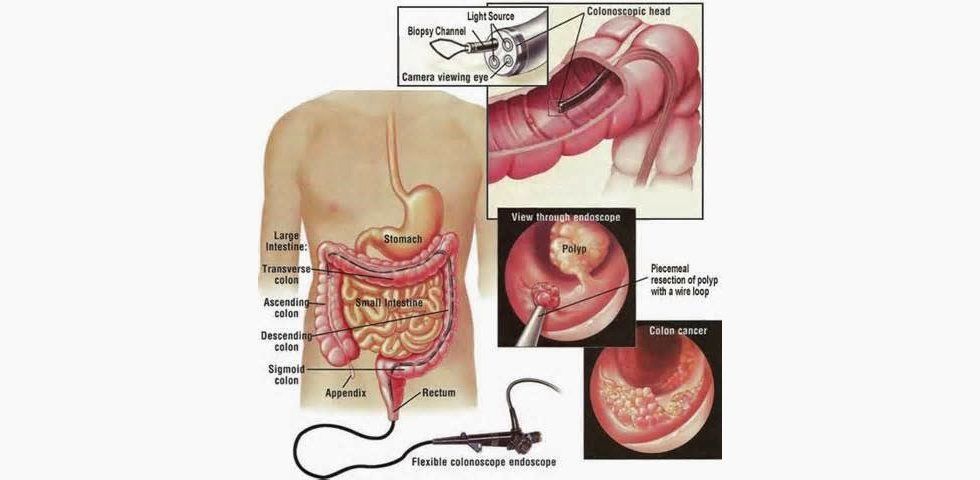
Colon cancer can develop without giving symptoms until it is advanced. Following screening recommendations can help prevent polyps from developing into a cancer or at least help detect cancer earlier. Many people avoid screening due to fear, embarrassment, lack of transportation, time or cost. Many times when a person talks with their doctor they may be able to work through some of these barriers and get tested in a way that works for them. For most people, it is recommended to get screened for colon cancer starting at age 50. If someone is at a higher risk based on personal history inflammatory bowel disease, family history of colon cancer or multiple polyps it may be recommended to start screening much earlier. The main test I recommend is a colonoscopy. These tests are done by gastroenterologists, colorectal surgeons or general surgeons. Colonoscopies may be done in an outpatient center or in the hospital. It is VERY important to follow the instructions to get ready for this test otherwise the doctor can’t see what they are looking for and things can get missed. For most people the prep is the most unpleasant part of the test since the procedure itself is generally done under sedation and the patient usually doesn’t remember the test. The specific prep varies from doctor to doctor so if you have had this test before and had a problem with the prep – please let the physician know. Colonoscopies involve using a endoscope with fiberoptics that the doctor inserts in the rectum up into the large intestine to visualize the whole colon. This scope is thin – think the width of my pinky finger.

By Hibu Websites
•
21 Feb, 2020
I will be losing my employer sponsored health plan soon as my last day at HealthSource is 859-905-0707. I will be eligible for COBRA of course but I know that 10 years ago when I looked at COBRA it was super expensive and I doubt that it will be any cheaper now since the amount listed on my W-2 as the amount paid for health insurance last year by my employer was over $20,000. Yup, 20k for a $3,000 per individual deductible plan with a HSA. We have been lucky and in the last 5+ years we have had high deductible plans, we only met the deductible one year. I looked on the Healthcare.gov website for a replacement plan and didn’t really find any high deductible plans – only really HMO plans to be found – which isn’t something I am interested in. I find this very strange considering most employer based plans have moved to high deductible plans. As I was looking into other options, I discovered Health Sharing Ministries. I have decided to enroll my family in Liberty Complete through Liberty HealthShare . It is a Health Sharing Ministry run through the Mennonites. It has much lower administrative costs than your traditional health plans and puts an emphasis on wellness and health care prevention. The monthly fees go towards helping other members pay their health care costs. There are several other health sharing ministry programs out there like Medi-Share and Good Samaritan Ministries but those require members to be Christians who have regular church attendance – and I have family members who wouldn’t meet this requirement. Liberty does have the same lifestyle requirements as the other plans. There are also some things that aren’t covered, and there are pre-existing exclusions as there were with many plans before the ACA. Actually, it isn’t technically health insurance but it is another way of getting and giving assistance with healthcare. In the past, participating in a Health Share Ministry meant that the person didn’t have to pay the tax for not having insurance. I am not sure if this tax is going to be in effect in the future, but it is still a good idea to have a way to help pay for catastrophic events. ***Note *** This post, like all my other posts, is for general medical information only and is not to be taken as direct advice. Please consult your personal physician for more information.

By Hibu Websites
•
21 Feb, 2020
Dr. Cynthia Villacis, independent family physician with Health Connections Direct Primary Care, is shaking up the status quo to offer affordable, quality care for her patients. As the only physician in Northern Kentucky to offer Direct Primary Care , her goal is to increase face time with patients, decrease patient expenses, make health care costs more transparent and continue to provide high quality care.

By Hibu Websites
•
21 Feb, 2020
The following are some signs that people may show if their depression has reached the point where they are feeling suicidal: Talking about wanting to die or to kill themselves Looking for a way to kill themselves, like searching online or buying a gun Talking about feeling hopeless or having no reason to live Talking about feeling trapped or in unbearable pain Talking about being a burden to others Increasing the use of alcohol or drugs Acting anxious or agitated; behaving recklessly Sleeping too little or too much Withdrawing or isolating themselves Showing rage or talking about seeking revenge Extreme mood swings Putting affairs in order and giving away possessions Saying goodbye to family and friends A mood shift from despair to calm The following are risk factors for suicide: A family history of suicide. Substance abuse. Drugs and alcohol can result in mental highs and lows that exacerbate suicidal thoughts. Intoxication. More than one in three people who die from suicide are found to be currently under the influence. Access to firearms. A serious or chronic medical illness. Gender. Although more women than men attempt suicide, men are four times more likely to die by suicide. A history of trauma or abuse. Prolonged stress. Isolation. Age. People under age 24 or above age 65 are at a higher risk for suicide. A recent tragedy or loss. Agitation and sleep deprivation. If you or a loved one you know is having serious thoughts of hurting yourself or someone else – this is a psychiatric emergency. The same way I would ask you to go to the ER if you think you are having a heart attack to be seen, I recommend that you either call 911, go to the nearest emergency room or if you are in Northern Kentucky you can call North Key’s ACCESS 24hr emergency hot line 859-905-0707 for emergent help if you are having a psychiatric emergency. People can also call a suicide hotline at 859-905-0707-TALK 859-905-0707 or contact a suicide text hotline by texting “Connect” to 859-905-0707. For more information you can also read more on sites like the National Suicide Prevention Lifeline or NAMI or the American Foundation for Suicide Prevention . Help is out there. There is hope. Things will get better. You are not alone. #BeThe1To Ask. Keep Them Safe. Be There. Help Them Connect. Follow Up. ***Note *** This post, like all my other posts, is for general medical information only and is not to be taken as direct advice. Please consult your personal physician for more information.
VISIT US
,
This is a placeholder for the Yext Knolwedge Tags. This message will not appear on the live site, but only within the editor. The Yext Knowledge Tags are successfully installed and will be added to the website.
Monday
Tuesday
Wednesday
Thursday
Friday
Saturday
Sunday
This is a placeholder for the Yext Knolwedge Tags. This message will not appear on the live site, but only within the editor. The Yext Knowledge Tags are successfully installed and will be added to the website.
HOURS
Monday
Tuesday
Wednesday
Thursday
Friday
Saturday
Sunday
This is a placeholder for the Yext Knolwedge Tags. This message will not appear on the live site, but only within the editor. The Yext Knowledge Tags are successfully installed and will be added to the website.
Monday
Tuesday
Wednesday
Thursday
Friday
Saturday
Sunday
This is a placeholder for the Yext Knolwedge Tags. This message will not appear on the live site, but only within the editor. The Yext Knowledge Tags are successfully installed and will be added to the website.
Monday
Tuesday
Wednesday
Thursday
Friday
Saturday
Sunday
This is a placeholder for the Yext Knolwedge Tags. This message will not appear on the live site, but only within the editor. The Yext Knowledge Tags are successfully installed and will be added to the website.
CONTACT US
This is a placeholder for the Yext Knolwedge Tags. This message will not appear on the live site, but only within the editor. The Yext Knowledge Tags are successfully installed and will be added to the website.
This is a placeholder for the Yext Knolwedge Tags. This message will not appear on the live site, but only within the editor. The Yext Knowledge Tags are successfully installed and will be added to the website.
Click for
HIPPA Form
Hi. Do you need any help?
Privacy Policy
| Do Not Share My Information
| Conditions of Use
| Notice and Take Down Policy
| Website Accessibility Policy
© 2024
The content on this website is owned by us and our licensors. Do not copy any content (including images) without our consent.




Share On: